Nexavar Maintenance Improves Survival for Patients with AML Subset
Patients with a subset of acute myeloid leukemia may have improved survival rates and lower risk of relapse with Nexavar maintenance.
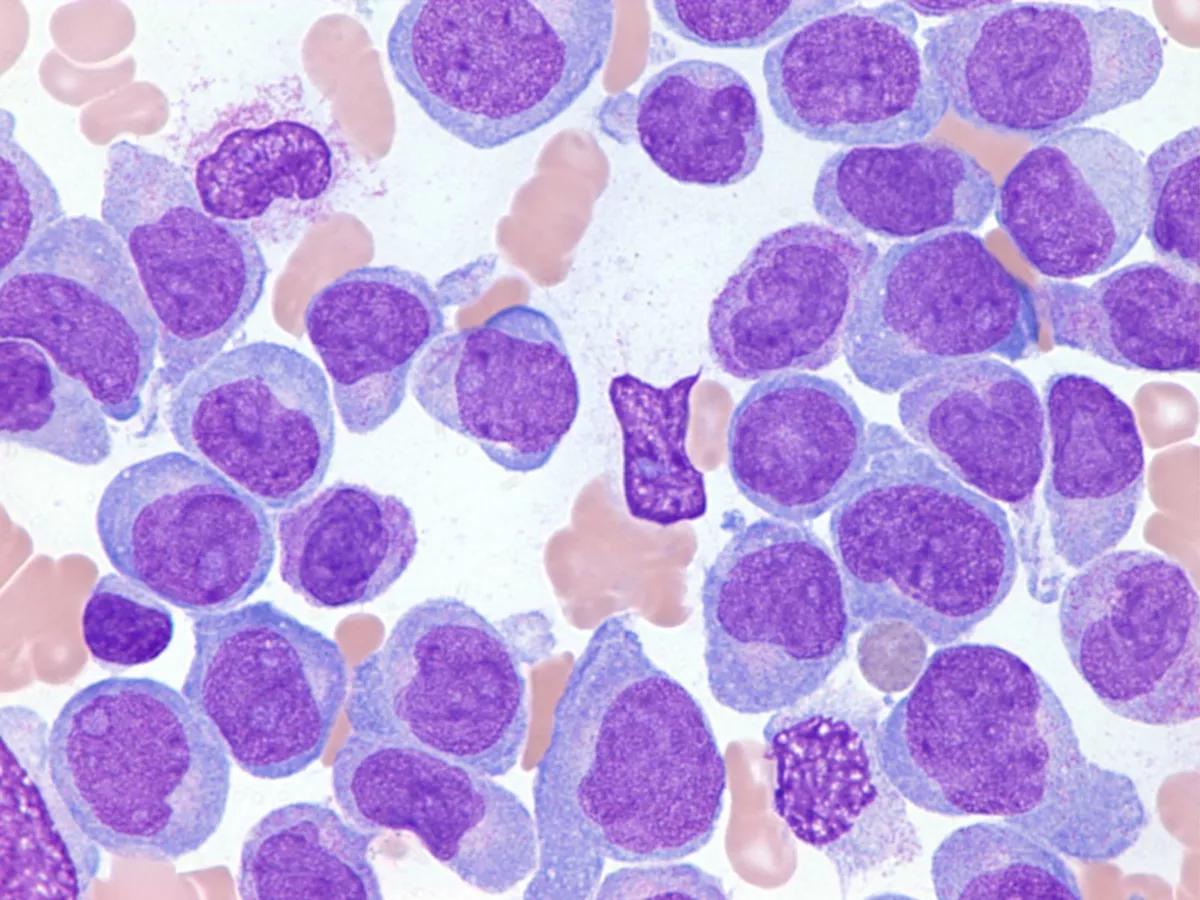
Long-term follow-up maintenance treatment with Nexavar (sorafenib, an oral chemotherapy drug) has been shown to improve survival for patients with FLT3 internal tandem duplication (FLT3-ITD, a frequent molecular abnormality) acute myeloid leukemia undergoing allogenic hematopoietic stem-cell transplantation (HSCT, a bone marrow transplant).
Nexavar maintenance after transplantation, according to a study published in The Lancet, not only improves long-term survival, but it also reduces relapse without an increase in late complications for patients with FLT3-ITD acute myeloid leukemia undergoing allogenic HSCT.
FLT3-ITD is a mutation that happens in about 25% of adults with acute myeloid leukemia, which causes shorter periods of remission and leads to higher rates of relapse compared with patients who are FLT3-negative, as the authors noted in the study. They found that allogenic HSCT improves survival rates for patients, but because leukemia relapses are common, the authors advise that implementing Nexavar is beneficial.
In the study, there were 202 total patients in the phase 3 trial randomly assigned across two groups. One group had a total of 100 patients and received Nexavar maintenance. The second group had a total of 102 patients and were placed in the non-maintenance control group. Of the patients who used Nexavar before transplantation, there were 59 patients in the Nexavar maintenance group and 57 patients in the control group. However, the authors emphasized that the 59 patients who used Nexavar before transplantation required dose modifications because of side effects, including 42 dose reductions, 12 dose interruptions, and five discontinuations.
According to the results of the study, 15 patients in the Nexavar maintenance group and 37 patients in the control group experienced relapses. The median time for relapses after transplantation was 11.9 months and 6.5 months for the Nexavar maintenance and control groups, respectively. In particular, eight patients in the Nexavar maintenance group relapsed approximately 12 to 24 months after transplantation, whereas 17 patients in the control group relapsed approximately six months after transplantation.
The median follow-up after transplantation for the Nexavar maintenance group was 21.3 months, in which survival improvements and relapse prevention began to show, as the authors found.
“Our results showed that the benefit derived from (Nexavar) maintenance after transplantation was sustained substantially beyond the end of treatment, with a five-year overall survival of 72% for patients in the (Nexavar) group and 55.9% for patients in the control group,” said the study authors.
According to the authors, Nexavar was administered to patients approximately 30 to 60 days after transplantation and was continued until day 180. Regarding relapse, the study results established that the two-year cumulative incidence (measure of occurrence of new disease during a period) of relapse was 11.9% in the Nexavar maintenance group and 31.6% for patients control group. This meant patients receiving Nexavar maintenance could reduce their risk of early relapse.
In the study’s follow-up analysis, “the long-term benefit of (Nexavar) maintenance after transplantation in improving relapse was sustained substantially beyond the end of treatment,” said the authors. After the follow-up analysis, the authors found that the five-year cumulative incidence of relapse was 15% for patients in the Nexavar maintenance group and 36.3% for patients in the control group.
For more news on cancer updates, research and education, don’t forget to subscribe to CURE®’s newsletters here.
‘Mommy Doesn’t Have Hair Right Now’: Receiving a Cancer Diagnosis as a Young Mother
October 28th 2021On this episode of the “Cancer Horizons” podcast, CURE® contributor Amanda Ferraro describes what it was like to receive a cancer diagnosis at 28 years old with a 3-year-old child and discusses the importance of mental health for cancer survivors.
Listen
‘Attitude is Everything’ When Dealing with Cancer
February 11th 2021This week on the “CURE Talks Cancer” podcast, we spoke with Nicole Schulz, who was diagnosed with acute myeloid leukemia at the age of 14, about how her life changed as a result of her treatment and why she now lives life to the fullest.
Listen