Patients With CLL Could Also Face Autoimmune Complications, Expert Says
Autoimmune diseases in patients with CLL are separate from CLL, which calls for different treatments.
Autoimmune complications “occur very commonly for people with CLL,” which is important for patients and caregivers to know, an expert told CURE®.
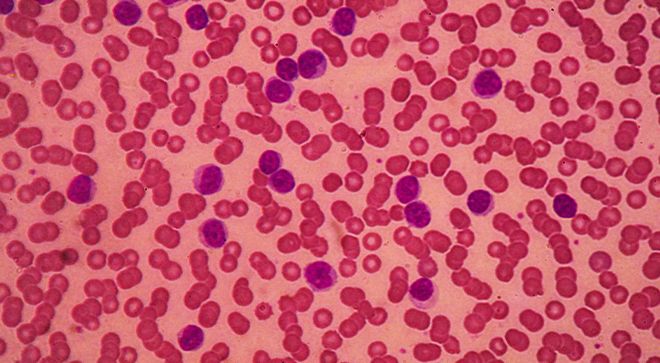
Chronic lymphocytic leukemia (CLL) is a slow-growing cancer in which higher levels of lymphocytes, a type of white blood cell, are located in the bone marrow, according to National Cancer Institute.
Autoimmune complications are diseases that cause the immune system to attack a patient’s own body, and CLL increases the potential for this attack, in which it is most common for the immunse system to target a patient’s red blood cells or platelets, explained Dr. Kerry Rogers, a physician and associate professor in the division of hematology at the Ohio State University Comprehensive Cancer Center — Arthur G. James Cancer Hospital and Richard J. Solove Research Institute.
Rogers presented about autoimmune complications in patients with CLL during the CURE® Educated Patient CLL Summit on Oct. 28.
Autoimmune diseases that are common among patients with CLL may include autoimmune hemolytic anemia and immune thrombocytopenia (ITP) and are treated differently than CLL, despite looking similar, said Rogers.
“(Autoimmune diseases are) actually separate from the CLL, which not a lot of people (understand),” Rogers noted. “I think it’s important that people know about this, so (that) if they do experience it, they have some basis for understanding it.”
Because autoimmune diseases are different than CLL, Rogers noted that it can be difficult for other types of healthcare professionals to diagnose.
“It’s a condition that is sometimes not diagnosed properly by non-hematologists, especially autoimmune hemolytic anemia, (which) can be very confusing to diagnose for ER physicians and even internists sometimes … (and) surgical specialists,” Rogers said.
She emphasized that if people with autoimmune diseases have more background knowledge, then they can help their healthcare professionals detect it sooner, especially if “something is changing with their blood counts, like anemia or a low platelet count, so that the other physicians can also think through, like, ‘Is this happening?’ and order appropriate testing. Sometimes since it’s rare — not in CLL patients, but in the general population — it’s something where I think knowing about this can help people ask appropriate questions about if this could be something that’s happening to them.”
Regarding treatment options for autoimmune diseases, Rogers said that one option is “problematically” high doses of Prednisone, which is an oral steroid drug that reduces inflammation and immune system responses. Another treatment option is Rituxan (rituximab), which Rogers noted is also a type of treatment for CLL.
“It does actually treat the CLL a little bit too and (Rituxan) is a drug that can be used in the treatment of CLL. But in this case, it’s not being used as a CLL treatment, it’s being used as a treatment for the autoimmune condition ITP,” she said. “These are immunosuppressants that are used to treat these conditions. In cases where standard immunosuppressants don’t work or the CLL also needs treatment, then treating the CLL will be a part of the treatment too.”
When patients with CLL develop an autoimmune disease, they could experience several symptoms.
“The major one that is most common is autoimmune cytopenia. So autoimmune hemolytic anemia can cause severe anemia, in fact, quite quickly, so people develop anemia quite rapidly, and usually, people will feel extremely fatigued, feel short of breath with any exertion, including walking to the bathroom, walking up the stairs, people will be too tired to leave their house, get out of bed to go to work or do normal activities,” Rogers said.
She also noted that red blood cell breakdown could also lead to alarming symptoms, including yellowing of the skin and the whites of the eyes and dark urine, which are caused by the breakdown product from the red blood cells.
A major symptom “so many people don’t notice” is bruising and bleeding easily, according to Rogers. “This can include something as simple as getting a giant bruise from something minor, like banging your hand on a doorframe and your whole hand is purple,” she said.
If patients with CLL and autoimmune diseases experience any of these symptoms or symptoms that interrupt their daily quality of life, Rogers urged them to meet with their hematologist oncologist immediately.
“The main advice I would offer is (to) make sure you understand exactly what you’re getting treatment for and what it’s supposed to accomplish, because I find a lot of times people get really confused between understanding what’s going to improve their autoimmune condition versus what’s supposed to improve the CLL,” said Rogers.
For more news on cancer updates, research and education, don’t forget to subscribe to CURE®’s newsletters here.